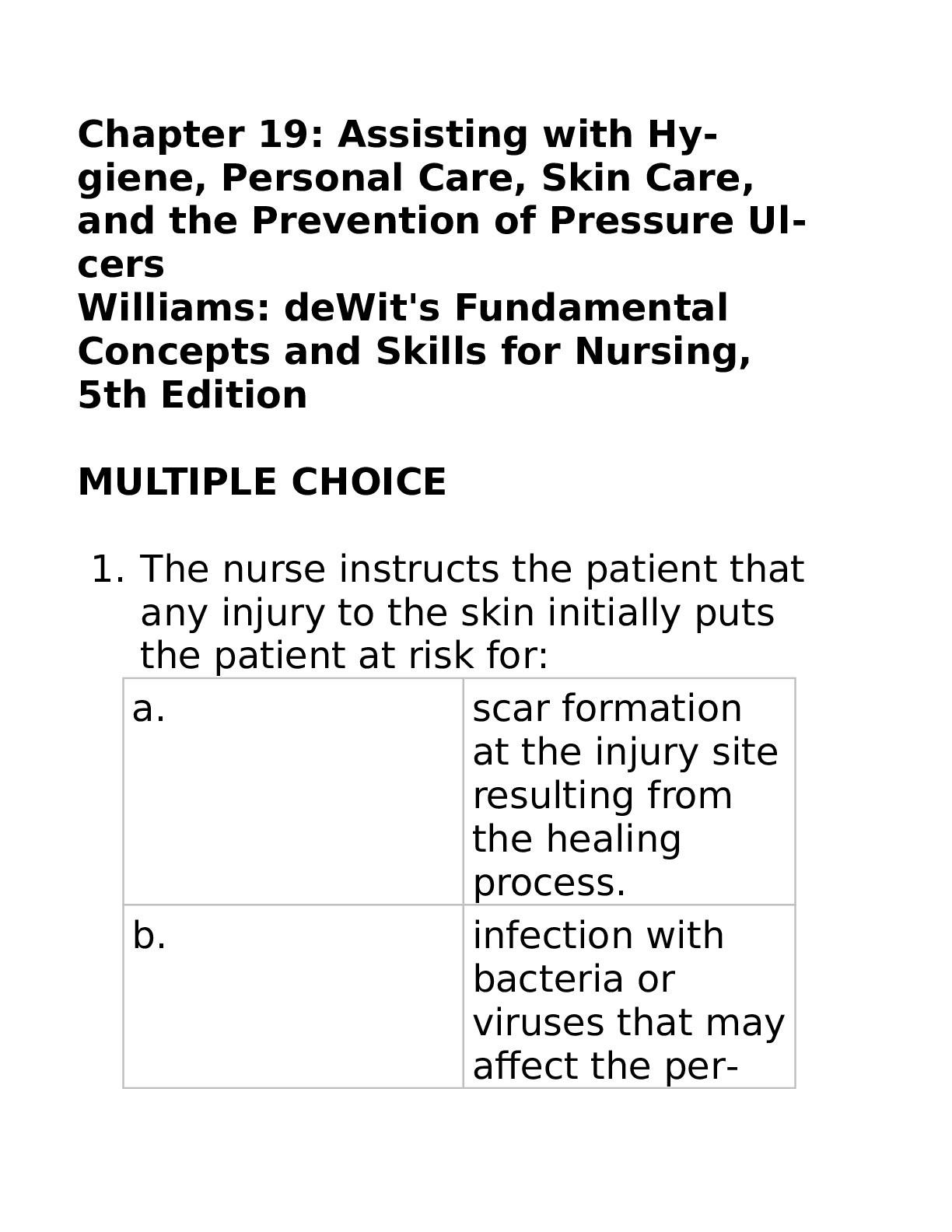
1. The nurse instructs the patient that
any injury to the skin initially puts
the patient at risk for:
a. scar formation
at the injury site
resulting from
the healing
process.
b. infection with
bacteria or
viruses that may
affect the person
systemically.
c. loss of sensation
caused by damage
to the
nerves in the
area.
d. loss of body fluids
and an upset
in the fluid and
electr
...[Show More]
1. The nurse instructs the patient that
any injury to the skin initially puts
the patient at risk for:
a. scar formation
at the injury site
resulting from
the healing
process.
b. infection with
bacteria or
viruses that may
affect the person
systemically.
c. loss of sensation
caused by damage
to the
nerves in the
area.
d. loss of body fluids
and an upset
in the fluid and
electrolyte balance.
2. When the patient returns from the
physical therapy department, he is
diaphoretic and his skin is flushed
but cool. Nursing intervention in
this situation should be for the
nurse to:
a. call his primary
care provider
about the
amount of exertion
in physical
therapy.
b. suggest the patient
walks
slowly in the hall
to “cool down.”
c. offer additional
fluids to replace
those lost
through normal
cooling.
d. place a light
cover over the
patient to prevent
his chilling.
3. During an admission assessment to
a skilled care facility, the nurse
notes that a 76-year-old man is thin
and unsteady on his feet and has
dry flaky skin on his arms and legs.
An appropriate hygiene goal for
this patient is that the:
a. patient will
shower daily on
an independent
basis by the end
of 1 month.
b. nurse will give a
tub bath or full
bed bath daily.
c. patient will
shower or tub
bathe with assistance
twice a
week.
d. patient will tub
bathe or shower
with assistance
daily.
4. In assessing the skin condition of
an older adult patient, the nurse
notes that, over the sacral area,
there is a 2 cm × 3 cm area that is
reddened, does not blanch around
the perimeter, and is open at the
center. The most effective documentation
would be:
a. “Patient has
stage II ulcer on
sacrum. No
blanching of
perimeter.”
b. “Reddened area
over sacrum,
skin open in
center.”
c. “Pressure ulcer
on sacrum. Massaged
with no
improvement in
color.”
d. “2 cm × 3 cm
reddened area
on sacrum with
open center.
Does not
blanch.”
5. When instructing a nursing assistant
about hygiene needs of a frail
older adult patient, the nurse correctly
educates the nursing assistant
to:
a. “Use warm, not
hot, water and
be sure the
room is warm
beforehand to
avoid chilling.”
b. “Put bath oil in
the tub and use
plenty of soap to
really clean the
patient’s skin
while she is in
the tub.”
c. “Use brisk drying
and an alcohol
rub to close
the patient’s
pores and prevent
heat loss
after the bath.”
d. “Completely dry
the patient’s
skin and apply a
mild moisturizer.”
6. An important factor to consider
when assessing the hygiene needs
of a patient is that:
a. the patient
knows best what
is needed in his
hygiene routine.
b. the routine of
the agency will
determine when
the patient is
able to bathe.
c. hygiene is not
as important as
other needs of
the patient.
d. the patient may
not have the
same hygiene
practices as the
nurse.
7. What nursing interventions related
to hygiene are appropriate for a patient
who has had a recent stroke
that caused right-sided (dominant)
paralysis and inability to speak?
a. Perform a full
bed bath, brush
and floss his
teeth, and give
him a good back
massage.
b. Encourage the
patient to use
his nondominant
hand to wash
his face, brush
his teeth, and
perform other
hygiene activities
with assistance
as necessary.
c. Set up a washbasin
and supplies,
tell the patient
to wash
what he can,
and provide privacy
for the patient
to do what
he can.
d. Teach a family
member to give
a full bath so
that the family
member will be
able to care for
the patient at
home.
8. The patient most at risk for a pressure
ulcer would be:
a. a 46-year-old
man in traction
for a fractured
femur, who exercised
regularly
before his accident
and is alert
and oriented.
b. a 54-year-old
overweight man
who is unconscious
from a
stroke, has a urinary
catheter in
place, and has
been incontinent
of liquid
stool since a
feeding tube
was placed.
c. a 72-year-old
man admitted
for elective
surgery to replace
his hip
joint, who was
an avid bowler
and gardener
before his hip
disease slowed
him down.
d. an 84-year-old
man with
Alzheimer disease
who is pacing
in the halls
and who is incontinent
of
urine if not toileted
every 2
hours.
[Show Less]